Kelly Bryan donated 70 per cent of her liver to Muhammad Khan.
An anonymous living liver donor helped the UHN Transplant Program achieve a North American first with an innovative living liver donor exchange or “swap” that saved the lives of two failing liver patients, with the potential to save many more.
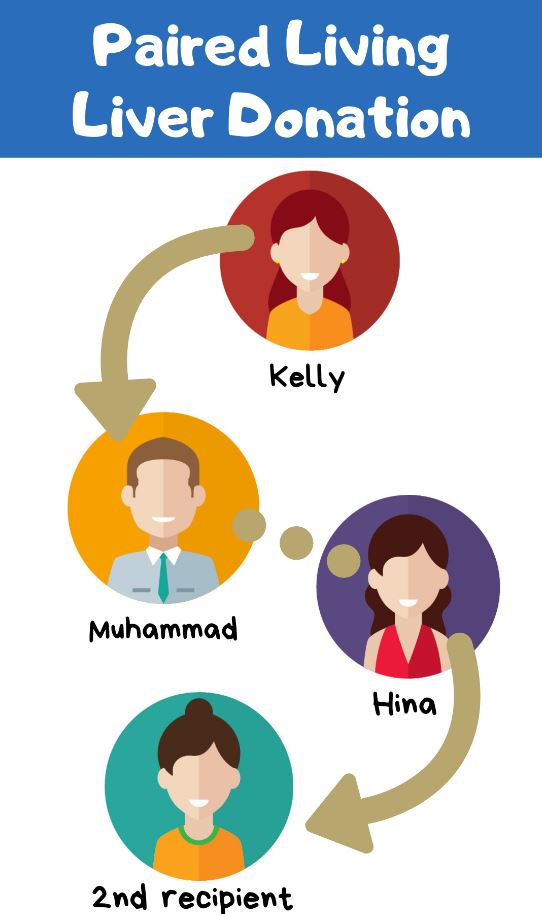
Kelly Bryan, a 38-year-old mother of three children, generously donated 70% of her liver to an adult stranger who needed a liver transplant. At the same time, that recipient’s wife donated more than half of her liver to another stranger to save her husband’s life, as her blood type was not compatible with her husband’s.
Kelly is a rare universal blood type O-negative, meaning she can donate blood to anyone. Organ donors must have a compatible blood type with the recipient. Only about 7% of the population has O-negative blood.
Kelly’s anonymous living liver donation to a dying patient allowed the transplant team to maximize the benefit of this extraordinary gift.
They did this by setting up a liver paired exchange donation. Living donors in a paired-organ donation or paired exchange trade recipients who have incompatible blood types, effectively creating two new compatible pairs.
In this instance, Kelly, the first donor, donated anonymously to a recipient she did not know, whose wife then agreed to anonymously donate a portion of her liver to another patient waiting for a transplant and chosen by the medical team. In this way, each recipient was able to receive an organ compatible with his or her blood type.
“I wanted to donate to a stranger because although they’re not my friend or family member, they’re still someone else’s friend, family, loved one and they deserve the gift of a new liver and new life,” says Kelly, who after her surgery felt especially moved to know that her recipient was thriving with a new liver.
Muhammad Khan, 54, is the recipient of Kelly’s generosity and portion of her liver. He was “totally shocked” when he received the diagnosis of non-alcoholic liver cirrhosis in 2017 while he was in Emergency because he was having difficulty breathing.
“To my donor, I would like to say that I have the deepest regards for you. I appreciate what you did from the depth of my heart. I salute you for doing such a tremendous job. For coming forward and helping me,” he said, adding that he is grateful to be able to see his two sons, 16 and 27 years old, finish school, get married, do well in their chosen fields, and lead happy lives.
Muhammad’s wife, Hina Khan, 49, is the second living donor who gave a portion of her liver to a stranger so that her husband could receive a liver transplant: “It was important for me to save my husband’s life. That is why I was willing to donate a part of my liver to somebody. At the same time, it was saving two people’s lives. I want more people to hear my story, and come forward, so they will also help each other.”
The recipient of Hina’s donation has chosen to remain private, and is doing well.
The four simultaneous surgeries took place on July 9, 2018 over 12 hours in total, with four operating rooms, and a team of 28 staff and surgeons. In total about 100 staff and physicians looked after the pairs before, during after the surgeries.
Dr. David Grant, University Health Network (UHN) transplant surgeon, and the liver transplant team had been waiting for about a year for the opportunity to save two lives simultaneously.
He explains that the first anonymous living donor gift benefits two recipients right away, and allows those on the deceased donors’ list to move up two places.
He points out that every year in Ontario, 50-100 people die while waiting for a liver transplant. Almost 300 people are on the waiting list for a liver in Ontario.
“That’s why it is so important to shout out to the world how life-changing and important this gift is,” says Dr. Grant, adding, “I have the utmost admiration for living donors.”
Zubaida Mohamed, Transplant Co-ordinator, Living Donor Liver Program, UHN Transplant, is a vital resource for living donors as they are tested and evaluated for suitability.
“Potential living donors feel they have a moral obligation to help someone in need simply because they can do it when they are healthy and alive,” says Zubaida. “They believe in random acts of kindness without repayment of any kind.”
Kidney paired exchanges – in which the recipients “swap” donors to receive blood compatible kidney transplants – have been successfully co-ordinated and extensively performed for the past 15 years. But exchanges involving a liver donation are far more rare.
Paired liver exchanges have been performed mainly in Korea and Hong Kong, with no published reports of them being done in Europe or North America.
Living liver donation is a riskier procedure than a living kidney one, with a 0.3% donor risk of death and a 30% risk of complications after an adult to adult donation, with the larger right liver lobe. This is what both donors in this paired exchange donated.
The livers of both the donor and recipient grow back to full size approximately three months after the surgery.
Evaluating these donors, and ensuring their safety, takes a highly co-ordinated and committed team of nurses, physicians, co-ordinators, social workers, ethicists and psychiatrists.
“This is a team effort. It can’t be done without a first-rate team,” emphasizes Dr. Grant.
Founded and fuelled by philanthropic support, UHN’s Centre for Living Organ Donation, part of the Transplant Program, is setting the gold standard in discoveries, treatment, and care for patients with end-stage kidney and liver disease who receive the gift of living donation.
In 2018, UHN Transplant performed 188 liver transplants, with 42 of them being adult living liver donor transplants. This makes it the second largest liver transplant program in North America. In addition, the UHN program also performed 12 transplants on children at the Hospital for Sick Children from living liver donors.
